Outlook on Nursing

The Growing Demand for Registered Nurses
The demand for nurses isn't a new issue, but it is coming to a critical juncture. Aging Baby Boomers – about 73 million of them – will all be over age 65 by 2030. As one of the largest generational cohorts in history, their transition into old age - and the accompanying natural progression of age-related conditions and chronic diseases - is creating a surge in demand for healthcare services. At the same time, nearly 1 million Registered Nurses (RNs) are expected to retire by 2030, leaving no relief in sight for the already-strained US nursing workforce.
These are just a few of the reasons for the nursing shortage, which is a complex and convoluted issue. One thing is sure – without a comprehensive solution, the current pipeline of newly licensed RNs will not meet the growing need.
Increasing the Number of RNs in the Field
With fewer than 205,000 newly licensed RNs entering the field in 2022 – the deficit to fill current and future job openings is enormous. So, how do we increase the number of new entry-level RNs? It begins with enrollment.
Pathways to Nursing
Newly licensed RNs – who have passed the National Council Licensure Examination for Registered Nurses (NCLEX-RN) – can prepare for licensure via several different accredited enrollment pathways.
- Bachelor of Science in Nursing (BSN) from a US college or university
- Associate Degree in Nursing (ADN) from a community college or vocational school
- Diploma in Nursing from a hospital or medical center program
- Graduation from a comparable international program
The BSN has long been associated with better patient outcomes and is recommended as the preferred degree for entry into nursing practice by organizations such as the American Nurses Association (ANA), American Association of Colleges of Nursing (AACN), and Institute of Medicine (now the National Academy of Medicine). BSN graduates comprised nearly 40% of the newly licensed nurse cohort in 2022, with ADN graduates following closely at almost 33%. The remaining approximately 27% is made up of international students (11%), repeat domestic candidates (15%), and diploma graduates (1%).
A landmark 2010 report on The Future of Nursing by the Institute of Medicine set the bar for the healthcare industry as a whole to increase the proportion of nurses with a BSN to 80% by 2020. Though that goal hasn't been reached on the national level, it remains a guidepost that hospitals, health systems, and professional organizations continue to strive for.
BSN Enrollment Trends
As the industry-preferred degree for entry-level RNs, growth in BSN enrollments seems like a promising trend – according to the AACN, enrollment more than tripled from 2001 to 2021. It continued its more-than-steady growth until 2022 when BSN programs experienced their first decline in 20+ years. While slight, it's concerning - given that the growth of the previous years hasn't proven enough to significantly impact shortages in the field. Even more concerning, over 65,000 qualified applications for entry-level BSN programs were turned down in 2022, further limiting the pool of potential new RNs.
Universities aren't turning down the opportunity for enrollment growth without good reason; the complexity of educating pre-licensure nurses creates limitations to expansion that can be difficult to overcome.
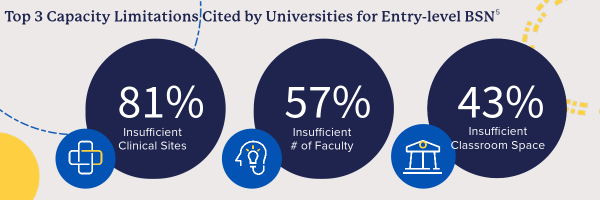
Insufficient Clinical Sites
Lack of sufficient availability of clinical placement sites was the most cited reason schools gave for turning away qualified applicants in an AACN survey in Fall 20225, with over 80% reporting it as a reason and over 40% reporting it as the most important reason.
Clinical placement experiences provide pre-licensure nursing students the opportunity to apply the knowledge and skills learned in the classroom in a real-world healthcare setting and are crucial to developing practice readiness in new nurses.
Insufficient # of Faculty
Nursing faculty shortages also constrain program capacity. AACN's annual survey on faculty vacancies found an overall faculty vacancy rate of 8.8% in 2022—85% of those vacancies required or preferred a doctoral degree.
The faculty shortage creates a vicious cycle – a lack of nurse educators spawns a shortage of new nurses, reducing the number of nurses who could eventually earn advanced degrees and become nurse educators. While the scale is smaller at the graduate level, the number of applications turned down for graduate programs is equally troubling for that very reason.
"Given the persistent shortage of nurse faculty, AACN remains concerned that more than 10,000 applications were turned away from graduate programs, which may further limit the pool of potential nurse educators. "
Insufficient Classroom Space
Lack of physical space to accommodate students and faculty, while cited by slightly less than half of survey respondents, remains a significant barrier. It's not just classrooms - office space for additional faculty members is also a consideration. Even more important are simulation labs, which play a vital role in teaching hands-on nursing skills.
Until enough universities can solve the issues constraining their nursing program capacity, potential new nurses will continue to be turned away, potentially delaying or ending their pursuit of a nursing career.
The Appeal of a Career in Nursing
There is obviously no shortage of career opportunities for aspiring RNs, one of the single largest occupations nationally, with slightly higher than average growth projected by the Bureau of Labor Statistics (BLS) to 2031. There is also no shortage of reasons to pursue a career in nursing.
- Job Security - The surplus of current and future opportunities (and the deficit of newly licensed RNs to fill them) provides a level of job security many other fields don't offer.
- Flexibility - Nurses can work in various roles and locations, including hospitals, clinics, physicians' offices, schools, research facilities, and more. Depending on the role, nurses may have the option to work part-time or full-time, with a wide variety of shift schedules.
- Opportunity for Growth - Nursing offers many personal and professional growth opportunities through direct patient care, education, and/or leadership. Professional advancement can be achieved through formal degrees or certifications and specialized professional development.
- Competitive Compensation - In May 2022, the median annual pay for registered nurses was $81,220, significantly more than the median annual wage for all workers of $46,310. While salaries vary depending on factors like education, experience, and geographic location, nursing offers the opportunity for a competitive salary.
- Personal Fulfillment - For many, nursing is a calling and a chance to make a positive impact on the lives of others. Nurses provide care, support, and comfort to patients during their most vulnerable times, which can be incredibly rewarding.
The positive career outlook and appeal of nursing have even spurred the growth of university programs geared specifically towards career changers – the accelerated second-degree Bachelor of Science in Nursing (ABSN). Enrollment in these programs comprised 11% of entry-level BSN enrollments in 2022 and 20% of graduates from Fall 2021 to Summer 20225. These accelerated programs only take 11-18 months to complete, speeding the entry of new BSN-prepared nurse graduates into the field.
Keypath partners are overcoming the challenges that limit capacity in entry-level BSN programs with the Distance Accelerated BSN. Learn more.
Challenges in the Nursing Workforce
With an inadequate number of new RNs entering the workforce, the upcoming exodus from nursing becomes even more problematic. As previously mentioned, nearly 1 million Registered Nurses (RNs) are expected to retire by 2030, and they aren't the only ones exiting the workforce. An analysis of a national survey of registered nurses compiled by researchers at the Project for Middle Class Renewal (PMCR) at the University of Illinois at Urbana-Champaign and the Illinois Economic Policy Institute (ILEPI) in 2022 found that 51% of surveyed nurses were considering leaving the profession in the next 12 months.
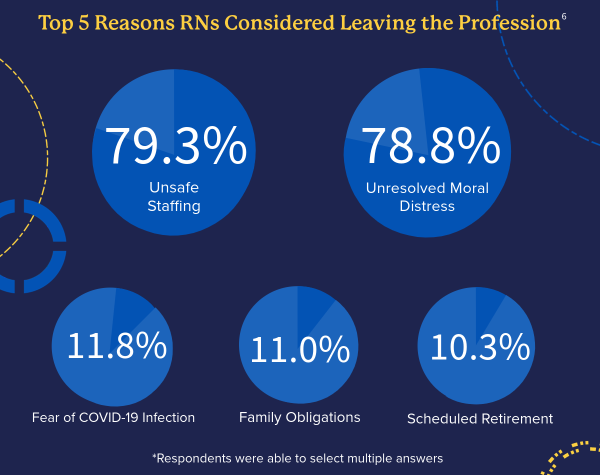
Why are they leaving? The primary reasons, cited by over 75% of the respondents, are unsafe staffing and moral distress.
The survey analyzed in the report was conducted by the nonprofit organization Nurses Take DC from October to November 2021, during the "Great Resignation," therefore reflecting the impact of the COVID-19 pandemic on health professions - and likely the discontent of the workforce at large.
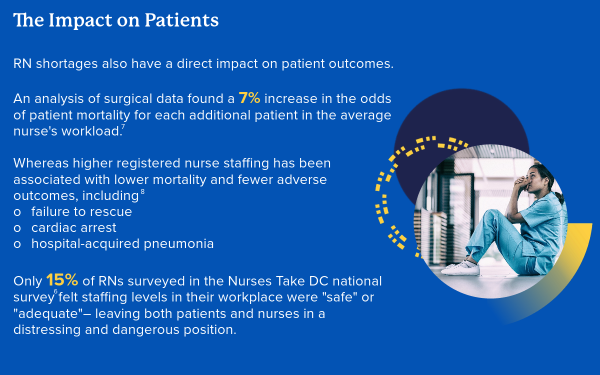
According to the 2023 NSI National Health Care Retention & RN Staffing Report, in 2022, hospitals were able to add back 4.17% (142,375) of the RNs they lost during the Great Resignation, lowering the national nurse vacancy rate by 1.3%. While any upswing is helpful, the average hospital RN vacancy rate remains at 15.7%, and the turnover rate is at 22.5%. Turnover – which encompasses both those leaving for new nursing roles and those leaving the field entirely - has a tremendous cost, and not just in actual dollars. Turnover also creates a burden on the remaining staff, diverting time, money, and resources to recruiting, hiring, and onboarding new team members and further contributing to strain and burnout.
Turnover is especially problematic in new hires, with nearly 75% leaving their roles within the first five years – 32.8% within the first year alone. Not every new hire is a recent graduate, but nurses with ten or fewer years of experience do seem to be feeling the most significant impact from problems in the workforce. An analysis of the 2022 National Nursing Workforce Survey in the Journal of Nursing Regulation, focusing on burnout, stress, and the impact of the COVID-19 pandemic, found that nurses with ten or fewer years of experience reported a higher frequency of negative emotions or stress than their more experienced colleagues, including feeling "emotionally drained, used up, fatigued, burned out, or at the end of their rope." They left the workforce at a higher rate (3%) than the overall average for all RNs (2.7%) during the pandemic, and of those remaining, 15.2% reported plans to leave the field in the next five years.
The effort being expended in higher education to combat nursing shortages by expanding nursing program capacity and educating more new entry-level RNs falls flat if a significant number of those nurses don't stay in the profession.
How can hospitals and health systems onboard and develop new graduate nurses in a way that increases their resilience and nurtures embeddedness in the profession? How can universities support the preparation of new graduate nurses to enhance their practice readiness and help ensure a seamless transition to practice? And most importantly, how can universities and hospitals develop meaningful academic-practice partnerships to overcome the broad scope of challenges the nursing workforce is facing?
True solutions can't just address one or two of the challenges facing the nursing workforce and nursing education – they must address the bigger picture. Only comprehensive and collaborative solutions - bridging nursing education and healthcare - will make an impact.
Overcoming the limitations to educating more new entry-level RNs
Nursing programs need to be able to expand their capacity to graduate more new entry-level RNs (especially at the BSN level) and to do so in a manner that cultivates diversity and inclusion. The biggest hurdle, clinical placements, requires the support of hospitals and health systems – and a cultural and structural shift to develop student placement as a future employee pipeline. Cultivating student placements as future employees and colleagues can create a deeper connection between students and the existing workforce and provide a head start to onboarding.
Transitioning new entry-level RNs into practice efficiently and effectively
Streamlining the transition between university programs and the workforce and increasing the practice-readiness of new nurse graduates creates efficiencies in onboarding and orientation, enhances their ability to practice independently, and helps to ease the burden on the current workforce. Developing alignment between universities and hospitals on key elements for entry-level nursing practice, with a clear system for reliable and informative competency tracking, can help bridge the academic-practice gap for an effective transition to practice.
Promoting Embeddedness to Improve Retention
Setting the stage early to help new entry-level RNs feel confident, included, and supported should make them more likely to stay - not just in their roles, but in the field. Embedding them in their future workforce while still completing their education provides the opportunity for streamlined entry into their new career, equipped with the skills and knowledge they need to be successful.
It's imperative to break the cycle of nursing shortages - for the sake of nurses and for the sake of the patients whose lives they touch. Meaningful academic-practice partnerships, with the right resources and support to recognize and reach the common goal, provide a sustainable, long-term solution that will transform the nursing workforce.
Keypath is committed to bridging the gap between hospitals, universities, and students with meaningful academic-practice partnerships that provide sustainable solutions to nursing workforce challenges. Learn more.
Sources
- Bureau of Labor Statistics, US Department of Labor, (2023, September 6) Occupational Outlook Handbook, Registered Nurses, at https://www.bls.gov/ooh/healthcare/registered-nurses.htm [visited October 19, 2023].
- Lightcast™, [accessed February 28, 2023].
- National Council of State Boards of Nursing, Inc, (2022) Exam Statistics & Publications, NCLEX Pass Rates, at https://www.ncsbn.org/public-files/NCLEX_Stats_2022-Q4-PassRates.pdf [visited July 13, 2023].
- Campaign for Action, (2022, March 9) Welcome to the Future of Nursing Dashboard/Dashboard Secondary Indicators, at https://campaignforaction.org/resource/campaign-dashboard-indicators/ [visited October 19, 2023].
- 2022-2023 Enrollment and Graduations in Baccalaureate and Graduate Programs in Nursing. Washington, DC: American Association of Colleges of Nursing.
- Project for Middle Class Renewal (PMCR) at the University of Illinois at Urbana-Champaign and the Illinois Economic Policy Institute (ILEPI), (2022, June 23) Registered Nursing in Crisis, at https://illinoisepi.files.wordpress.com/2022/06/pmcr-ilepi-registered-nurses-in-crisis-final.pdf
- Aiken LH, Clarke SP, Sloane DM, Sochalski J, Silber JH. Hospital Nurse Staffing and Patient Mortality, Nurse Burnout, and Job Dissatisfaction. JAMA. 2002;288(16):1987–1993. doi:10.1001/jama.288.16.1987
- Kane RL, Shamliyan T, Mueller C, Duval S, Wilt TJ. Nurse staffing and quality of patient care. Evid Rep Technol Assess (Full Rep). 2007 Mar;(151):1-115. PMID: 17764206; PMCID: PMC4781632